Tuberculosis
Q: What is tuberculosis?
A: Tuberculosis (TB) is a disease caused by the bacterium Mycobacterium tuberculosis. TB has been documented in humans from the dawn of civilization going by various names like consumption, white plague, kshaya vyadhi etc. TB can affect any organ of the body, but lungs are most commonly affected.
Q: How serious is the problem of TB in current times globally and in our country?
A: Even today, TB accounts for diseases with one of the highest mortality rates, especially in the developing and under-developed countries. In 2020, an estimated 15 lakh people died from TB around the world. Due to the devastating COVID-19 pandemic, TB deaths increased for the first time in over a decade, due to diversion of resources and difficulty in access to regular healthcare. India is a high TB burden country with an estimated 26 lakh people developing tuberculosis disease annually.
Q: How does TB spread?
A: Tuberculosis is an airborne disease and spreads from person to person through droplets nuclei. When a person with active tuberculosis disease of the lungs either coughs, spits, or sneezes, the germs are thrown into air suspended in the droplets. Any person in close distance (household contacts and close contacts) who inhales these droplets gets infected.
Q: Who is at risk of developing active TB?
A: People of every socio-economic status are at risk of developing the disease in our country. Although TB can occur in any age group and both sexes, those between 20-40 years are commonly affected. A person can develop active disease when the nutrition intake is poor, there is physical or mental stress, tobacco, alcohol or illicit drugs usage, diabetes, chronic lung, kidney and liver diseases, other immunocompromised conditions and HIV infection.
Q: What are the features of TB?
A: TB is insidious in nature. Any cough with or without sputum production lasting for more than 2 weeks, blood on coughing, low grade fever, weakness, tiredness, loss of appetite, and unintentional weight loss, warrants a check up with a healthcare professional for TB.
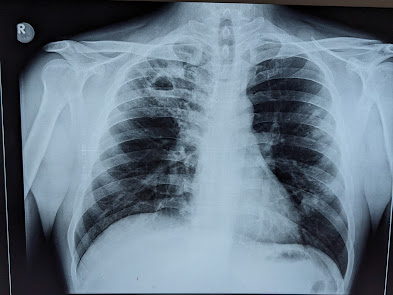
Q: How is TB diagnosed?
A: For the diagnosis of lungs TB (Pulmonary Koch's disease), a chest x-ray, and most importantly, sputum tests are required. In some cases where there is no sputum production, a CT scan of chest and Bronchoscopy maybe warranted. For TB affecting other organs like lymphnodes, pleura, abdomen, brain etc., specific tests like needle aspiration and biopsy maybe required.
Q: Is effective treatment available for TB?
A: Tuberculosis is a treatable and curable disease. The right regimen of anti-TB drugs (Rifampicin, Isoniazid, Ethambutol, Pyrazinamide), taken for the prescribed duration of minimum 6 months, achieves high cure rates. Drug compliance, nutritious diet, and a regular follow up with the treating physician is very important for achieving cure. Timely anti tubercular therapy also helps prevent spread of infection to other healthy persons.
Q: Are anti-TB drugs available in our country?
A: Yes, anti-TB drugs are available everywhere in our country in both government and private sectors.
Q: Are there are any treatment options in traditional and alternative systems of medicine?
A: There is no scientific evidence for any effective treatment options in complementary and alternative medicine, or traditional systems of medicine for tuberculosis.
Q: What happens if we don’t take proper treatment for TB?
A: Without proper treatment, active TB disease can be fatal in 45% to 50% of HIV negative individuals, and 100% fatal in people living with HIV. Also, improperly treated TB can lead to the more dangerous drug resistant tuberculosis (MDR and XDR TB) which requires much longer treatment duration (~20 months) with multiple drugs (5-7 drugs).
Q: How can we prevent tuberculosis?
A: Tuberculosis can be prevented by maintaining a nutritious balanced diet, regular physical activity, avoiding alcohol, tobacco and illicit drugs usage, practicing cough etiquette, hand hygiene and most importantly, by timely identification and treatment of persons with active disease to break the chain of transmission. BCG vaccination for the newborns helps prevent the development of more serious forms of tuberculosis and needs to be given as per schedule. TB Preventive Therapy, wherein a single anti-TB drug (Isoniazid) or two drugs (Rifapentine and Isoniazid) are given for household contacts (family and caregivers) and close contacts of active TB patients, is also recommended.
Sources and further reading links
2. https://www.who.int/health-topics/tuberculosis#tab=tab_1
3. https://www.cdc.gov/tb/default.htm
4. https://www.nhs.uk/conditions/tuberculosis-tb/
5. https://www.healthline.com/health/tuberculosis#risk-factors





Comments
Post a Comment